Gastroenterology
About
A prompt and accurate diagnosis, top-quality endoscopic services, as well as targeted, effective and personalized treatments for patients with digestive diseases are our top priorities.
We focus on continuously improving our medical services. We achieve this thanks to our team’s passion for gaining scientific knowledge and our investment in the latest technical and theoretical training, our high-quality endoscopic equipment, and the holistic approach we take towards each of our patients.
We are passionate about innovation and progressing our medical field, thus we take part in research and clinical trials, and we train medical students and our new staff.
Welcome to the Department of Gastroenterology.
Dimitrios Giannakakis.
Small bowel capsule endoscopy
Endoscopic Ultrasound (EUS)
for the staging of upper digestive cancers, investigation/monitoring of submucosal digestive/cystic and other pancreatic tumors, diagnosis of stones and the investigation of extrahepatic bile vessel abnormalities.
Placement of bare metal stents

Drainage of esophageal varicose
Endoscopic hemostasis
Colonoscopy
ERCP
Percutaneous endoscopic gastrostomy (PEG)
Balloon dilatations
Cauterization
Polypectomy/EMR
Gastroscopy
The Department
The Department of Gastroenterology at the German Medical Institute (GMI) offers expert medical services, which cover a wide range of digestive diseases.
Part of our services focus on diagnosing and treating oncology patients, mainly patients with tumors in their digestive system.
With each visit to the department, you can experience our team’s expert medical training, and our holistic and personalized approach. We recognize the varied needs of each individual patient. Our team works on accurately diagnosing and effectively treating each of our patients. Our nursing and support staff are on hand to help you feel safe and at ease.
To provide the best possible medical services, we closely collaborate with other GMI departments, including the Department of Medical Oncology, Radiation Oncology, Radiology, Histopathology and Nuclear Medicine.
Our department is part of the weekly GMI Gastroenterology Oncology Board, where a multidisciplinary team comes together to ensure that the treatment plan we devise for each patient is optimal.
Services
The Department of Gastroenterology at the GMI offers a wide range of diagnostic and medical services on both a clinical and endoscopic level.
These include:
- Regular outpatient clinics, which operate daily. Here we take each patients' medical history and perform clinical examinations. These are followed by a consultation where we either diagnose a patient or recommend further testing. If necessary, medication is prescribed, and patients are scheduled for future visits, or referred to other specialists.
We also closely monitor patients with diseases of the upper and lower digestive tract, e.g., gastroesophageal reflux disease, gastritis, gastric/duodenal ulcers, inflammation or tumors in the digestive tract. We also closely monitor patients with diseases of the bile, bile ducts, pancreas, and liver, and provide biopsies when necessary. As part of our holistic approach to medicine, the department works with a clinical nutritionist and all the other paramedical services of GMI.
Patients with chronic inflammatory bowel diseases (e.g., Crohn's disease or ulcerative colitis) are also monitored and treated in the outpatient clinic. When deemed necessary, we offer infusions of biological agents in our day care unit.
- Our department also offers a wide range of endoscopic services using state-of-the-art equipment and our fully trained and qualified specialist staff.
With very few exceptions, endoscopies are performed using propofol and therefore are as painless as possible for our patients. Recovery is immediate after the procedure, and non-hospitalized patients can usually be discharged within a few minutes. Before leaving the center, they receive a detailed report with a record of their endoscopic images. In more complex cases and invasive endoscopic procedures, or whenever our medical team deems it necessary, patients can be admitted to the hospital ward.
More specifically, the Department of Gastroenterology offers the following endoscopic services:
- Gastroscopy (endoscopy of the esophagus, stomach, and duodenum) with or without collecting biopsies. For all patients, a biopsy for urease testing (direct diagnosis of Helicobacter pylori) is also performed during the examination.
- Colonoscopy (endoscopy of the colon and the terminal ileum) with or without biopsies.
- Polypectomy/EMR or removal of other benign or malignant tumors of the upper and lower digestive tract. The endoscopic removal of an early-stage cancer tumor is usually the only necessary treatment.
- Endoscopic hemostasis (treatment of gastrointestinal bleeding) via hemostatic clips, submucosal adrenaline injection, cautery or hemospray.
- Coagulation of angiodysplasias of the digestive tract using Argon-plasma.
- Band ligation of esophagus varices
- Balloon dilatations of esophageal, gastric, duodenal, ileal and colonic strictures.
- Placement of bare metal stents under fluoroscopy for treatment of esophageal strictures
- Percutaneous endoscopic gastrostomy (PEG) or change of PEG in patients who are unable to be fed orally.
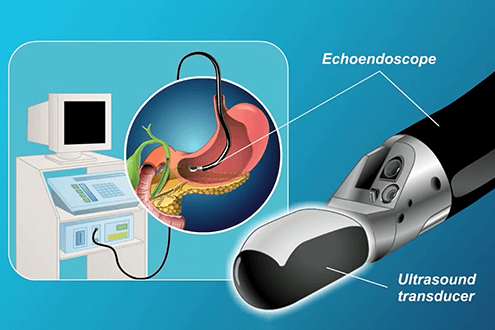
- Endoscopic Ultrasound (EUS) for the staging of upper digestive cancers, investigation/monitoring of submucosal gastrointestinal tumors and cystic pancreatic tumors, diagnosis of stones and the investigation of extrahepatic bile duct abnormalities.
- ERCP with sphincterotomy and the removal of stones from the bile duct/stenting of bile vessel stenoses.
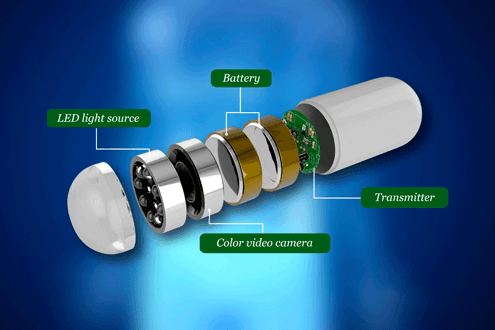
- Small bowel capsule endoscopy (investigation of iron deficiency anemia, suspected small bowel bleeding/tumor)
Our Team
The team at the Department of Gastroenterology is comprised of experienced doctors, who will explain your diagnostic and medical plan in detail during your consultation, and who will carry these plans out with your agreement. Monitoring patients with chronic diseases is carried out with great care and responsibility.
Dr. Dimitrios Giannakakis is the Director of the Department of Gastroenterology.

Equipment
The Department of Gastroenterology is equipped with the latest high-definition endoscopes, allowing for the best possible imaging and therefore most accurate diagnosis, leading to better medical care.
Our endoscopic towers have a supply of carbon dioxide, which is used in routine colonoscopies and other invasive endoscopic procedures. Due to the much faster absorption of this gas compared to regular air, the risk of complications during an endoscopy, as well as the feeling of abdominal pain after the end of the endoscopy, is significantly reduced, making the examination more pleasant for patients.
More specifically, the following gastroscopes and colonoscopes are used in our department:
- Routine gastroscopes
Olympus GIF-1100 HD
Olympus GIF-HQ190 HD
- Therapeutic gastroscope (large diameter)
Olympus GIF-1TH190
- Pediatric gastroscope
Olympus GIF-H190N HD
- Colonoscopes
Olympus CF-HQ1100DL HD
- Duodenoscope for ERCP (Endoscopic retrograde cholangiopancreatography)
Olympus TJF-Q190V
All the above endoscopes have additional image enhancement functions, such as:
- NBI (narrow band imaging)
This is an imaging technique for endoscopic diagnostic examinations, where light of specific blue and green wavelengths is used to enhance the detail of the mucosal surface. Mucosal lesions can therefore be better discerned and assessed.
- RDI (red dichromatic imaging)
This imaging technique enhances the visibility of deep vessels and sources of active bleeding. Endoscopic identification and therefore hemostatic treatment therefore made more easily and promptly.
- TXI (texture and colour enhancement imaging)
This imaging technique uses white light effects, improving the colour, brightness, and morphology of the mucosa, increasing the visibility and ease of detection of potentially suspicious tissue.
For endoscopic ultrasounds, we use the following endoscope:
- Olympus GF-UE190 RADIAL EUS
For the application of the small bowel endoscopic capsules, the following system is used:
- Olympus EC-10, MAJ-2029 (software ver. 3)
FAQs
During your medical consultation, your doctor will ask you about your medical history. This includes:
- Information on any medication you take, how long and how often you take it, and at what dosage (written or in photo form)
- Reports from other doctors you have visited
- Test results, such as blood tests, previous endoscopies, imaging tests, ultrasound scans, CT/MRI scans, etc.
Complete, accurate and timely information shared between patients and their medical team will help expedite the diagnostic process.
Due to our efforts to minimize the spread of SARS-CoV-2, a 24-hour COVID-19 rapid test is required before entry into our facilities.
During a gastroscopy a doctor checks your upper digestive tract (esophagus, stomach, duodenum: meaning the beginning of the small intestine). Common reasons why your medical team may recommend a gastroscopy are abdominal pain, discomfort and indigestion, anemia, dysphagia (difficulty swallowing), pain during swallowing, vomiting, digestive bleeding, unexplained weight loss, anorexia, or acid reflux disease that does not respond to treatment. Gastroscopies are also part of cancer screening programs.
A gastroscopy is usually scheduled ahead of time, except in emergencies for acute conditions or conditions that require a diagnosis on short notice. You must fast from the night before the examination, not consuming any food or fluids beforehand, to minimize the risk of these contents moving into the lungs, which can cause pneumonia.
You will be placed under moderate sedation (soft form of aneasthesia) to ensure you feel as comfortable as possible during the examination, using a peripheral intravenous catheter.
During a colonoscopy a doctor checks your lower digestive tract (colon and ileum). Common reasons why your medical team may recommend a colonoscopy are digestive bleeding, iron deficiency anemia, abdominal pain, a change in your bowel habits, or to monitor polyps or cancer. Colonoscopies are also an important part of cancer screening programs.
Colonoscopies are usually scheduled ahead of time as a lot of preparation is required. The stool in the bowel must be cleared so that it doesn’t obstruct your doctor’s vision when they are checking the mucosa (colonic and terminal ileum). This is usually achieved through 3-4 days of a specific diet, as well as with laxatives prescribed for the day before and in some cases for the day of the examination. All the steps you need to take will be given to you in writing, as well as explained to you during your consultation.
Just like for a gastroscopy, you will be placed under moderate sedation during the examination.
To check the bowel, the procedure requires air to be injected to prevent the walls from collapsing. This allows us to inspect the entire lumen (inside area) of the bowel. Air inside the bowel may cause some bloating and discomfort until it is expelled. As a rule, CO2 (carbon dioxide) is used as it is easier for the body to tolerate and it reduces discomfort after the examination, as CO2 is 250 times faster to absorb than regular air.
It is a common misconception that general anesthesia must be administered to undergo an endoscopy. General anesthesia is required for critical surgery, or surgery where a patient must be intubated. Our department only uses moderate sedation for endoscopies.
We do not recommend you use heavy machinery or drive for the rest of the day after being sedated. Therefore, we recommend you are accompanied to the center by someone who can then drive you home.
Our trained staff administer the medicaments which are warranted for a soft sedation. The team includes normally a gastroenterologists, and endoscopic nurses. However, we always have an anesthesiologist on site ready to intervene, if necessary, when performing these examinations.
The presence of an anesthesiologist throughout the entire examination is mainly required for patients with severe health problems, where there is an estimated higher risk for anesthesia-related complications.
The most common complications are:
Bleeding, which occurs in less than 1% of examinations and is most often caused by a polypectomy, with the removal of large polyps, or if a patient has a coagulation disorder. In this event, patients will notice either dark red or black blood and should notify their physician. Usually, the bleeding will occur immediately after the procedure. On very rare occasions, it can occur up to 14 days after the procedure.
Perforation, meaning the tearing of the wall of the intestine, is another possible complication with an extremely low probability. The risk of this occurring depends on each patient’s underlying condition. The existence of a bowel inflammation, bowel stenosis, old age, multiple health problems, adhesions from past surgery, bowel cancer, bowel ischemia, resection of polyps (larger than 1 cm), dilatation of stenoses and others such variables increase the risk of a perforation. A perforation commonly manifests with severe abdominal pain, nausea, fever, vomiting, or rectal bleeding. Treatment, depending on the circumstances, can be performed endoscopically on the spot, or surgically.
Post-polypectomy syndrome involves a localized inflammation, without perforation of the bowel, that can cause pain, tenderness, and a fever up to 5 days after a polypectomy. Typically, the onset is immediate, and it is treated with intravenous fluids, antibiotics, and bowel rest (no oral fluid or solid intake) for 1-3 days.
After the examination, you will be taken to the recovery room where you can lie down until you have fully recovered from sedation. Patients are supervised by a nurse throughout this process. If you feel abdominal pain or bloating, you should report this to a member of staff immediately. This discomfort is usually caused by excess air, and we encourage you to expel this. Recovery from the procedure is brief and any feelings of discomfort are rare and last for only a few minutes.
You will then be briefed by your medical team about the procedure and their findings. This is followed by a written report, printed images of the examination and any further recommendations whenever appropriate, including medication, follow-up examinations, laboratory/imaging tests or a future appointment for regular monitoring.
In the case where a biopsy or polypectomy was performed, histopathological results will be ready after a period of about 10-12 days. Once the findings are ready, your medical team will inform you immediately and if there are any pathological findings that require further investigation, they will offer recommendations for how to proceed.

Contact details
- (+357) 25 208 000
- [email protected]
- 1, Nikis Avenue 4108, Agios Athanasios, Cyprus
- Mon - Fri | 08:00 - 16:30



